Garrett Dempsey, PhD

Hola mi nombre es Garrett. Originally from Illinois I moved to San Diego to attend UCSD. Now at UC Berkeley in the lab of Andreas Stahl I am researching the role of tension in brown and beige adipose tissue development and function. Outside the lab you can catch me running, cooking, writing, and attempting to learn Spanish.
Also, I write for FoundMyFitness! Follow their page!
Education and Research
UC Berkeley, PhD Candidate, 2016-2022
Metacrine Inc, Research Associate, Nov 2015- June 2016
Receptos Inc., Associate Scientist, Feb 2015-Nov 2015
University of San Diego, Undergraduate, 2011-2015
Diyala Shihadih, PhD

I’m a PhD candidate in Metabolic Biology. I grew up in the bay area and earned my bachelor’s degree in Biochemistry and Molecular Biology at UC Davis. Currently, I am researching how lipid transport and metabolism are altered in disease states such as cancer and how these altered functions can be therapeutic targets.
Education and Research
University of California, Berkeley; PhD candidate; 2015-2022
University of California, Davis; Undergraduate 2011-2015
Awards and Fellowships
UC Berkeley Chancellor’s Fellowship recipient
2018 Outstanding Graduate Student Instructor
You can also find me on ResearchGate.
Peter-James H. Zushin, PhD
 Biological generalist turned metabolic biologist that is currently learning bioengineering techniques to further investigate the thermogenic adipose tissue niche in vivo. Since coming to the Stahl lab I have been involved in our CoQ, Fat-on-a-chip, and hyaluronic acid-based hydrogel for beige adipose tissue formation projects. My interests lie at the intersection of evolution, tissue development, and bioengineering techniques that can help investigate those topics!
Biological generalist turned metabolic biologist that is currently learning bioengineering techniques to further investigate the thermogenic adipose tissue niche in vivo. Since coming to the Stahl lab I have been involved in our CoQ, Fat-on-a-chip, and hyaluronic acid-based hydrogel for beige adipose tissue formation projects. My interests lie at the intersection of evolution, tissue development, and bioengineering techniques that can help investigate those topics!
Education and Research
UC Berkeley; Graduate Student (Ph.D); 2015-2022
Boston University; Graduate Student (M.A.); 2009-2012
University of Akron; Graduate Student (M.S.); 2006-2009
University of Akron; Undergraduate; 2001-2005
Awards and Fellowships
2018, Ruth L. Kirschstein NRSA Predoctoral Fellowship, NIH (NIBIB)
You can also find me on Research Gate.
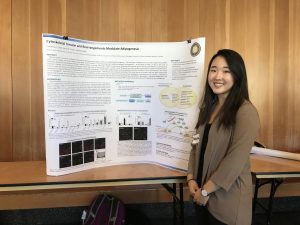
Ching-Fang Chang, PhD
 I see myself as a multidisciplinary biomedical biologist focusing on energy metabolism and stem cell biology. My goal is to find a practical intervention to effectively combat obesity and its associated metabolic disorders.
I see myself as a multidisciplinary biomedical biologist focusing on energy metabolism and stem cell biology. My goal is to find a practical intervention to effectively combat obesity and its associated metabolic disorders.
Education and Research
University of California, Berkeley; Postdoc; July 2014-2022



 Biological generalist turned metabolic biologist that is currently learning bioengineering techniques to further investigate the thermogenic adipose tissue niche in vivo. Since coming to the Stahl lab I have been involved in our CoQ, Fat-on-a-chip, and hyaluronic acid-based hydrogel for beige adipose tissue formation projects. My interests lie at the intersection of evolution, tissue development, and bioengineering techniques that can help investigate those topics!
Biological generalist turned metabolic biologist that is currently learning bioengineering techniques to further investigate the thermogenic adipose tissue niche in vivo. Since coming to the Stahl lab I have been involved in our CoQ, Fat-on-a-chip, and hyaluronic acid-based hydrogel for beige adipose tissue formation projects. My interests lie at the intersection of evolution, tissue development, and bioengineering techniques that can help investigate those topics! I see myself as a multidisciplinary biomedical biologist focusing on energy metabolism and stem cell biology. My goal is to find a practical intervention to effectively combat obesity and its associated metabolic disorders.
I see myself as a multidisciplinary biomedical biologist focusing on energy metabolism and stem cell biology. My goal is to find a practical intervention to effectively combat obesity and its associated metabolic disorders.
 Classical brown adipose tissue (BAT) is a unique type of adipose tissue that is composed of adipocytes with multilocular lipid droplets and a large amount of mitochondria, making it a highly metabolically active organ that is responsible for nonshivering thermogenesis both in neonate and adult humans. Brown adipocytes possess an unparalleled ability to generate heat due to the dissociation of electron transport chain respiration from ATP production through uncoupling protein 1 (UCP1). Brown adipocyte mitochondria also display an elevated capacity for substrate utilization. A major source of substrate is the β-oxidation of long chain fatty acids (LCFA), which can be taken up from the circulation via fatty acid transport proteins (FATPs) or can be generated from endocytosed lipoproteins through a process mediated in part by the scavenger receptors. The scavenger receptor (SR) family of transmembrane glycoproteins mediates the binding and uptake of a broad range of ligands in a variety of tissues. A defining member of the SR-B receptors is CD36, which has been shown to be required in a variety of tissues for the uptake of several hydrophobic molecules, including LCFA and the carotenoid lycopene. More recently, it was demonstrated that CD36 is required for the endocytosis of lipoproteins by both macrophages and BAT.
Classical brown adipose tissue (BAT) is a unique type of adipose tissue that is composed of adipocytes with multilocular lipid droplets and a large amount of mitochondria, making it a highly metabolically active organ that is responsible for nonshivering thermogenesis both in neonate and adult humans. Brown adipocytes possess an unparalleled ability to generate heat due to the dissociation of electron transport chain respiration from ATP production through uncoupling protein 1 (UCP1). Brown adipocyte mitochondria also display an elevated capacity for substrate utilization. A major source of substrate is the β-oxidation of long chain fatty acids (LCFA), which can be taken up from the circulation via fatty acid transport proteins (FATPs) or can be generated from endocytosed lipoproteins through a process mediated in part by the scavenger receptors. The scavenger receptor (SR) family of transmembrane glycoproteins mediates the binding and uptake of a broad range of ligands in a variety of tissues. A defining member of the SR-B receptors is CD36, which has been shown to be required in a variety of tissues for the uptake of several hydrophobic molecules, including LCFA and the carotenoid lycopene. More recently, it was demonstrated that CD36 is required for the endocytosis of lipoproteins by both macrophages and BAT. Discovering clinically relevant tactics to balance energy homeostasis and combat metabolic disorders such as obesity and diabetes is of the upmost importance. Brown adipose tissue (BAT) is a thermogenic organ that consumes energy substrates to generate heat through the mitochondrial uncoupling protein-1 (UCP1). The recent discovery that adult humans possess functional BAT and activating BAT can increase its uptake of circulating glucose and fatty acids suggests its potential therapeutic application on controlling glucose homeostasis and energy metabolism.
Discovering clinically relevant tactics to balance energy homeostasis and combat metabolic disorders such as obesity and diabetes is of the upmost importance. Brown adipose tissue (BAT) is a thermogenic organ that consumes energy substrates to generate heat through the mitochondrial uncoupling protein-1 (UCP1). The recent discovery that adult humans possess functional BAT and activating BAT can increase its uptake of circulating glucose and fatty acids suggests its potential therapeutic application on controlling glucose homeostasis and energy metabolism.